Keratoconus, an eye condition characterized by a bulging of the cornea, results in significant visual impairment for those affected. While the exact causes of keratoconus are still relatively unknown, researchers have made great technological advances in its treatment.
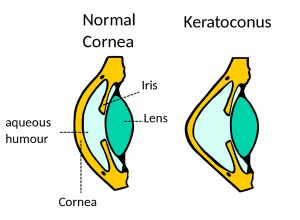
Keratoconus is an eye condition that results when the cornea, or outer lens of the eye, loses its dome-like shape. In people with keratoconus, the cornea becomes unusually thinned due to a weakening of protective fibers in the cornea. This weakening in the corneal fibers causes the cornea to lose its normal shape, and it begins to take on a cone-like, bulging form.
The exact cause of corneal thinning is not known. Keratoconus tends to be genetic, but it may also be caused by excessive eye-rubbing due to allergies or other environmental factors. The condition normally appears during adolescence or the early twenties, but it also may occur later in life. Researchers estimate that keratoconus affects 1 in 2,000 people, and affects men and women equally with no differences between races or ethnicities.
Keratoconus may cause significant vision problems in those affected. The shape of the cornea is essential to proper vision, and as the cornea loses collagen and thins, the vision may become distorted in a variety of ways.
The symptoms of keratoconus may come on suddenly or over a period of several years. The first symptoms are normally blurred vision that cannot be corrected with eyeglasses or contact lenses. As the condition develops, more significant vision problems may include:
Treatment of keratoconus has two main goals: One is to stop its progression and the other is to improve vision. Interestingly, treatments to improve vision, although not ideal, have been around for many years, whereas a treatment to stop keratoconus from progressing has only recently been approved in the United States. Prior to advanced research, the only treatment options available for keratoconus were Intacs, or plastic corneal inserts, and specialty contact lenses. While these methods can be effective in the early stages of keratoconus, they are unable to correct the significant visual impairment that occurs in more developed keratoconus cases.
A new treatment method called corneal collagen cross-linking, has recently been developed that has changed the lives of many patients with keratoconus. This new technology is simple, minimally-invasive, and can be performed in an office setting. It is extremely effective in stopping the progression of keratoconus, but has a very modest effect in improving vision.
Corneal cross-linking works by increasing the number of collagen crosslinks, or protective fibers, within the cornea. By limiting the deterioration of the cornea, corneal cross-linking works to halt the progression of keratoconus.
The second goal in the treatment of keratoconus is to improve vision. When vision can no longer be improved with glasses, the next step in treatment is fitting the patient with special contact lenses, such as a scleral lens that floats over the cornea with its periphery resting on the sclera. These lenses, in effect, regularize the shape of the cornea. If a patient has a hard time applying or removing a scleral lens, they may opt for a gas permeable contact lens which is smaller and is a good option for those with mild to moderate keratoconus. However, there are some patients whose keratoconus is too advanced to be treated with even these special contacts.
If contacts do not improve vision, Intacs may be used to treat keratoconus. These are arc-shaped plastic inserts that are implanted in the cornea outside the patient’s line of sight to flatten and reshape the cornea. The main goal of intacs is to prevent the need for a corneal transplant by strengthening the cornea enough to tolerate contact lenses. However, depending on the severity, the goal for intacs may vary. In some cases, vision can significantly improve to the point glasses or contact lenses may not be needed.
A corneal transplant is possible for patients with the most advanced type of keratoconus, who often have corneal scarring. Although traditional full thickness corneal transplants are more successful for keratoconus than for other cornea diseases, the procedure has recently improved. Partial thickness corneal transplants (DALK) now further improve outcomes due to lower risk of rejection. Thanks to new technology, partial thickness procedures allow surgeons to replace only the innermost layer of the cornea helping to lower the risk of rejection and recovery time for the patient when compared to a traditional transplant where the entire corneal tissue is replaced.
Make an appointment today at one of our eight convenient Atlanta-area locations.
Schedule an Appointment Online
Or call 678-381-2020